Myelocytes are a type of white blood cell that is normally not present in the peripheral blood. However, in certain conditions, such as bacterial infections, myelocytes may be released into the bloodstream, along with other immature cells like metamyelocytes and band neutrophils. This phenomenon is known as a “left shift,” and it indicates an increased demand for white blood cells to fight off an infection.
While a left shift can be a ueful diagnostic tool in identifying bacterial infections, an excess of myelocytes and metamyelocytes in the blood can also be a sign of a more serious underlying condition. High levels of these immature cells have been associated with increased mortality, particularly in patients with systemic inflammatory response syndrome (SIRS).
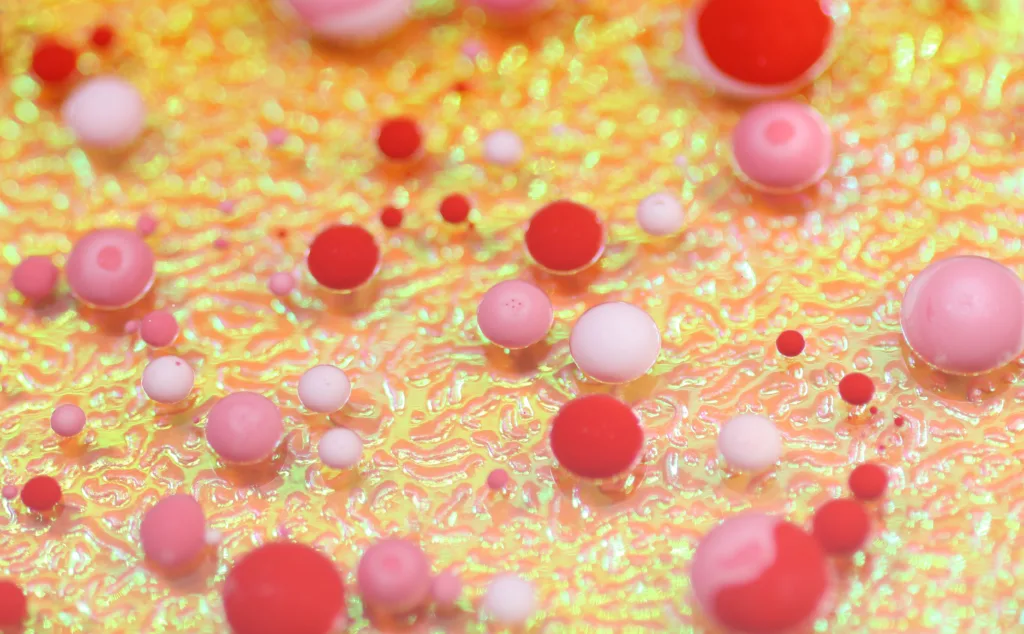
Neutrophils are a type of white blood cell that play a crucial role in the immune response to infection. They are derived from myeloid precursor cells in the bone marrow, and their differentiation progresses through several stages, including promyelocytes, myelocytes, metamyelocytes, and band forms, before producing mature neutrophils.
In normal circumstances, the bone marrow produces an appropriate number of mature neutrophils to meet the body’s needs. However, during periods of increased demand, such as during an infection, the bone marrow may release immature cells like myelocytes and metamyelocytes into the bloodstream to help fight off the invading pathogens.
While this response can be beneficial in the short term, a prolonged excess of immature cells in the blood can indicate a disturbance in the normal production and maturation of white blood cells. This can be caused by a variety of factors, including infections, inflammation, growth factor effects, marrow infiltration, and myeloid neoplasms.
While myelocytes and metamyelocytes can play an important role in the immune response to infection, an excess of these immature cells in the blood can be a sign of an underlying condition. Monitoring the levels of these cells can be a useful diagnostic tool, particularly in patients with SIRS, but further investigation may be required to determine the underlying cause of the left shift.
What Does It Mean When Myelocytes Are High?
When the levels of myelocytes are high in the blood, it usually indicates an abnormal increase in immature white blood cells that are yet to fully develop into mature cells. Myelocytes are a type of granulocyte that are formed in the bone marrow, and their increased presence in the blood is often an indication of a potential underlying medical condition.
This condition is often referred to as myelocytosis or myelocytic leukemia, and it can lead to the development of a wide range of symptoms including fever, fatigue, weakness, and increased susceptibility to infections. In some cases, high levels of myelocytes can also be an indication of an underlying bone marrow disorder or other serous medical condition.
It is important to note that high levels of myelocytes and metamyelocytes are associated with increased mortality, and therefore, prompt medical attention is necessary to determine the underlying cause and initiate appropriate treatment.
Can Infection Cause Myelocytes?
During bacterial infection, the bone marrow may respond by releasing more immature neutrophils, such as myelocytes, metamyelocytes, and band neutrophils, into the peripheral blood. This phenomenon is called ‘left shift’ and is a sign of a bacterial infection. The shortage of mature neutrophils in the peripheral blood during an infection leads to the release of these immature cells to fight aganst the invading pathogens. Therefore, the presence of myelocytes in the peripheral blood may indicate an ongoing bacterial infection. It is worth noting that left shift is not specific to bacterial infections and can also occur during other conditions, such as inflammation, trauma, and certain cancers.
Is Myelocytes In Blood Normal?
Myelocytes are a type of immature white blood cells that are not typically found in the peripheral blood of healthy individuals. The presence of myelocytes in the peripheral blood may indicate a variety of conditions, including infectious or inflammatory diseases, marrow infiltration, growth factor effect, and myeloid neoplasms. while myelocytes are not normal in peripheral blood, their presence can be an indication of an underlying health issue.
What Do Myelocytes Turn Into?
Myelocytes are a type of precursor cell that belongs to the myeloid lineage. These cells eventually differentiate into mature neutrophils, whch are a critical component of the immune system. As myeloid differentiation progresses, promyelocytes, myelocytes, metamyelocytes, and band forms are produced before the final maturation into neutrophils. Myelocytes are the second stage of development in this process and are characterized by a large, round nucleus with distinct chromatin clumps. After myelocytes, the cells further differentiate into metamyelocytes, which have a kidney-shaped nucleus and cytoplasmic granules, and then into band forms, which have a horseshoe-shaped nucleus. band forms mature into segmented neutrophils, which have a lobed nucleus and are fully functional in fighting infections.

Conclusion
An increase in myelocytes and metamyelocytes in the peripheral blood is often associated with systemic inflammatory response and bacterial infections. These immature cells are released due to a shortage of mature neutrophils and are not nomally present in the blood. The presence of myelocytes and metamyelocytes is a sign of left shift and is also associated with increased mortality. Therefore, it is essential to monitor the levels of myelocytes and metamyelocytes in patients with inflammatory conditions and bacterial infections to ensure appropriate management and improve clinical outcomes. Further research is needed to fully understand the mechanisms underlying the release of these immature cells and their role in disease progression.
