Plethysmography, or simply pleth, is the graphical representation of the pulse oximeter signal over time. It is a valuable tool in monitoring oxygen saturation levels in patients, especially those who are mechanically ventilated. However, not all plethysmographs are created equal, and it is important to know what a good pleth loks like to ensure accurate monitoring and diagnosis.
A good pleth should have a regular waveform with clearly defined peaks and troughs. The peaks correspond to the systolic phase of the cardiac cycle, while the troughs correspond to the diastolic phase. The amplitude of the waveform should be uniform and stable, indicating consistent blood flow to the tissue. A good pleth should also have a fast rise time, meaning that it reaches its maximum amplitude quickly, and a slow fall time, indicating a gradual decrease in blood flow during the diastolic phase.
In addition to waveform characteristics, a good pleth should also have a stable baseline. The baseline is the level of the waveform during the diastolic phase, when there is minimal blood flow. A stable baseline is important because it allows for accurate measurement of the pulse rate and oxygen saturation levels. If the baseline is noisy or fluctuates significantly, it can be difficult to determine the true pulse rate and oxygen saturation levels.
To ensure a good pleth, it is important to properly position the pulse oximeter sensor on the patient’s finger or earlobe. The sensor should be snug but not too tight to avoid restricting blood flow. The patient’s finger or earlobe should be warm and dry, as cold or wet skin can affect the accuracy of the reading. It is also important to avoid motion artifact, which can occur when the patient moves or the sensor is bumped, causing the pleth to become distorted or disappear altogether.
A good pleth is characterized by a regular waveform with clearly defined peaks and troughs, a uniform and stable amplitude, a fast rise time, a slow fall time, and a stable baseline. Proper sensor placement and minimizing motion artifact are also important factors in obtaining a good pleth. By understanding what a good pleth looks like, healthcare professionals can ensure accurate monitoring and diagnosis of patients’ oxygen saturation levels.
Understanding the Meaning of ‘Pleth’ on an ECG
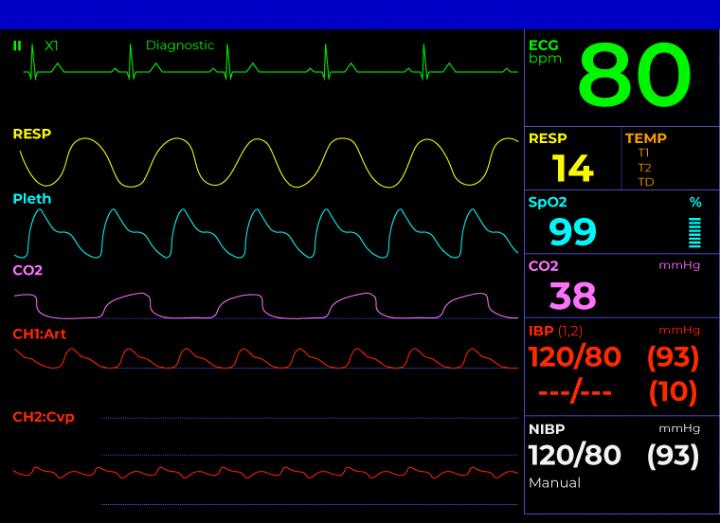
Pleth on ECG refers to the photoplethysmograph waveform that is generated by a noninvasive device called a pulse oximeter. The pleth waveform is a graphical representation of the pulsatile changes in blood volume in the peripheral tissues, which occur with each heartbeat. The waveform is derived from the absorption and reflection of light by the blood vessels in the fingertip, earlobe, or other peripheral tissue.
The pleth waveform is an important clinical tool that is used to monitor the oxygen saturation levels in the blood and the pulse rate. The waveform can also provide information about the patient’s cardiovascular status, such as the presence of arrhythmias or other abnormalities in the cardiac rhythm.
In addition, the pleth waveform can be used to assess a patient’s fluid responsiveness. This is done by analyzing the variability of the waveform durng respiratory cycles, which is measured as the pleth variability index (PVi). PVi provides a continuous noninvasive measure of the relative variability in the pleth waveform during respiratory cycles that may be used as a dynamic indicator of fluid responsiveness in select populations of mechanically ventilated adult patients.
To summarize, the pleth waveform on ECG is a graphical representation of the pulsatile changes in blood volume in the peripheral tissues, which can provide important clinical information about a patient’s cardiovascular and respiratory status, including their fluid responsiveness.
Source: youtube.com
Understanding the Meaning of Pleth on a Pulse Oximeter
A pulse oximeter is a non-invasive medical device used to measure the oxygen saturation level in a patient’s blood. The device works by shining a light through the patient’s skin and measuring the amount of light absorbed by the blood. The resulting signal is then displayed on the pulse oximeter screen.
One of the most prominent features on the pulse oximeter screen is the pleth, wich is short for plethysmograph. The pleth is a graphical display of the pulse oximeter signal over time. It shows the changes in the absorption of light as blood flows through the patient’s tissues.
The appearance of the pleth can vary depending on the patient’s clinical condition. A normal pleth will show a regular waveform with consistent peaks and valleys. However, in some cases, the pleth may be irregular or show fluctuations that indicate poor blood flow or low oxygen saturation.
The pleth can provide valuable information to healthcare providers about a patient’s condition. It can help them identify potential problems such as hypoxemia, hypovolemia, or poor perfusion. Additionally, monitoring changes in the pleth over time can help providers track a patient’s response to treatment.
The pleth on a pulse oximeter is a graphical display of the pulse oximeter signal over time. It can provide valuable information to healthcare providers about a patient’s condition and is an important tool in the management of patients with respiratory and circulatory problems.
What Is Considered a Normal Oximeter Level?
A pulse oximeter is a non-invasive medical device that measures the oxygen saturation level in a person’s blood. The oxygen saturation level is expressed as a percentage and is commonly referred to as SpO2. A normal SpO2 level is usually 95% or higher, which means that the blood is carrying enough oxygen to meet the body’s needs.
However, it is important to note that some people with chronic lung disease or sleep apnea may have a normal SpO2 level around 90%. If you are unsure about what your normal SpO2 level should be, it is best to consult with your healthcare provider.
It is recommended that individuals regularly monitor their SpO2 levels using a pulse oximeter, especially if they have a medical condition that affects their oxygen levels. If your home SpO2 reading is lower than 95%, it may be an indication of low oxygen levels in your blood. In such a case, it is important to contact your healthcare provider immediately for futher evaluation and treatment.
A good oximeter level is usually 95% or higher, but this may vary depending on individual circumstances. It is important to regularly monitor your SpO2 levels and consult with your healthcare provider if you have any concerns.
The Impact of an Oxygen Level of 94
Oxygen saturation levels are an important indicator of respiratory health. The normal range for oxygen saturation levels is between 95% and 100%. However, a level of 94% is still considered to be within a safe and healthy range for most individuals. It is important to note that oxygen saturation levels can vary based on a number of factors, including age, altitude, and underlying health conditions.
For individuals with lung problems, such as chronic obstructive pulmonary disease (COPD) or asthma, oxygen saturation levels may be lower than average. In these cases, a healthcare provider may recommend supplemental oxygen to help maintain adequate oxygen levels in the blood.
It is also worth noting that oxygen saturation levels can fluctuate thoughout the day and may be affected by factors such as exercise, sleep, and medication use. If you have concerns about your oxygen saturation levels, it is always best to discuss them with a healthcare provider.
While an oxygen saturation level of 94% may be slightly lower than average, it is still considered to be within a safe and healthy range for most individuals.
Normal Range of P Wave
The P wave is an important feature of an electrocardiogram (ECG), which reflects the electrical activity associated with atrial depolarization. It is characterized by its amplitude and duration, which are key indicators of normal atrial function.
The normal range for P wave amplitude is typically less than or equal to two and a half small squares (0.25 mV). In other words, the height of the P wave should not exceed 2.5 mm in a standard ECG recording. This range is important to observe because an increase in P wave amplitude can indicate atrial hypertrophy or enlargement, while a decrease in amplitude can indicate atrial conduction abnormalities.
Similarly, the normal range for P wave duration is typically less than or equal to tree small squares (0.12 s). This range is important to observe because a prolonged P wave duration can indicate conduction abnormalities in the atria, such as atrial flutter or fibrillation.
The normal range for P wave amplitude is less than or equal to 0.25 mV, and the normal range for P wave duration is less than or equal to 0.12 s. These ranges are important to observe in order to detect any abnormalities in atrial function and to aid in the diagnosis of various cardiac conditions.
Source: cardiacdirect.com
Normal P Wave Value
In an electrocardiogram (ECG), a P wave is a small, upward deflection that represents the electrical activity of the atria of the heart. It is an important component in determining the overall health and function of the heart. The normal P wave value is considered to be 80 milliseconds.
It is important to note that deviations from this value can indicate underlying cardiac conditions, such as atrial fibrillation or atrial flutter. Therefore, it is essential to interpret the P wave in conjunction with other ECG components, such as the PR interval and QRS complex, to get a comprehensive understanding of the heart’s electrical activity.
In addition, it is important to understand that normal values may vary slightly depending on the individual and the specific circumstances of the ECG. For example, a P wave value of 70-90 milliseconds may be considered within the normal range in some cases.
Understanding the normal P wave value is crucial in detecting and diagnosing potential cardiac abnormalities, and should be evaluated in conjunction with other ECG components in order to povide an accurate assessment of heart function.
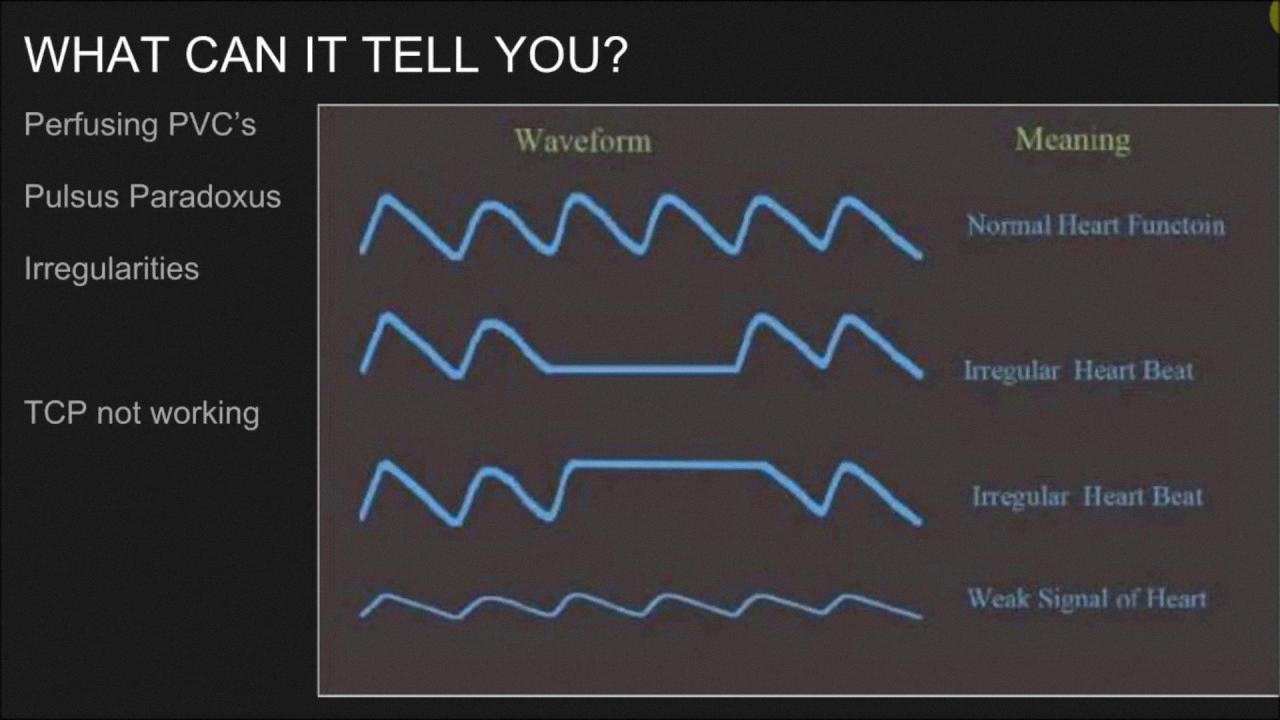
Interpreting a Pleth
A pleth waveform is a graphical representation of the pulse waveform, which displays the changes in blood volume during each cardiac cycle. This waveform is generated by a pulse oximeter, which is a non-invasive monitoring device used to measure the oxygen saturation level in the blood. The pleth waveform shows the pulse rate, pulse amplitude, and the overall shape of the pulse waveform.
The pulse rate is the number of times the heart beats per minute, and it is represented by the frequency of the wave. The pulse amplitude is the height of the wave and indicates the strength of the pulse. The overall shape of the wave can provide information about the regularity of the heartbeat and the presence of any abnormalities.
Pleth waveform analysis can be useful in detecting irregular heart rhythms such as atrial fibrillation, where the heart beats in an irregular pattern. It can also be used to monitor patients during surgery or after a heart attack to ensure that the heart is functioning properly.
The pleth waveform provides valuable information about the pulse rate, pulse amplitude, and overall shape of the pulse waveform. It is a non-invasive monitoring tool that can help detect irregular heart rhythms and monitor the heart’s function in vaious clinical settings.
What Is Considered a Normal Perfusion Index?
A perfusion index (PI) is a measure of the strength of a person’s pulse and blood flow to their extremities. The normal range of PI is from 0.02% to 20%. A good perfusion index varies depending on the individual’s health status and medical condition. However, a PI reading above 1% is generally considered good and indicates strong blood flow and pulse strength.
If the PI reading is at or blow 0.4%, it indicates weak pulse strength, and the oximeter reading may be unreliable. Poor perfusion can be caused by peripheral artery diseases, diabetes, obesity, blood clots, and other medical conditions.
It’s important to note that a perfusion index reading should be interpreted in conjunction with other vital signs, such as heart rate, blood pressure, and oxygen saturation, to get a complete picture of a person’s health status. A healthcare provider will use this information to make an accurate diagnosis and determine the appropriate treatment plan.
A good perfusion index reading is above 1%, indicating strong blood flow and pulse strength. However, it’s essential to consider other vital signs and medical conditions to make an accurate assessment of a person’s health status.
The Effects of Low Perfusion
Low perfusion is a medical condition that occurs when there is a decrease in the amount of blood flow to the peripheral tissues of the body. This condition can occur due to a variety of reasons, such as shock, heart failure, or hypothermia. In low perfusion, the amount of oxygen and nutrients delivered to the tissues is reduced, which can cause damage to the tissues and organs.
One of the ways low perfusion is detected is through the use of medical devices, such as pulse oximeters, which measure the oxygen saturation level in the blood. However, when there is low perfusion, the signal detected by the sensors may be reduced, leading to inaccurate readings. This can be a problem, as accurate readings are crucial for monitoring the patient’s condition and administering appropriate treatment.
Low perfusion can also affect the accuracy of other medical devices, such as blood pressure monitors and electrocardiograms (ECGs). In thee cases, the reduced blood flow can cause a decrease in the amplitude of the signals, making it difficult to obtain accurate readings.
To address the issue of low perfusion, medical device manufacturers have developed technologies that can compensate for the reduced signal strength. For example, some pulse oximeters use algorithms that can adjust the signal to account for low perfusion, resulting in more accurate readings.
Low perfusion is a condition where there is a decrease in blood flow to the peripheral tissues of the body, which can cause inaccurate readings from medical devices. Medical device manufacturers have developed technologies to address this issue and provide more accurate readings for patients.

Dangerously Low Oxygen Levels
A dangerously low oxygen level is a condition in which the amount of oxygen in the blood falls below normal levels, which can lead to hypoxia, a potentially life-threatening condition. The normal range for oxygen saturation is between 95% and 100%, which means that the blood is carrying enough oxygen to meet the body’s needs.
If the oxygen saturation levels drop below 92%, it is recommended to contact a health care provider as it may indicate the onset of hypoxia. This condition occurs when the body does not receive enough oxygen to function properly, leading to symptoms such as shortness of breath, confusion, and fatigue.
If the oxygen saturation levels fall to 88% or lower, immediate medical attention is necessary as it can be life-threatening. Some of the common causes of dangerously low oxygen levels include lung diseases, heart problems, anemia, and hyperventilation.
It is important to note that oxygen saturation levels can be measured uing a pulse oximeter, a non-invasive device that clips onto the finger, toe, or earlobe. This device measures the amount of oxygen in the blood and provides a reading within seconds. Monitoring oxygen saturation levels is crucial for individuals with underlying medical conditions and those who are at risk of developing hypoxia.
A dangerously low oxygen level is a condition in which the amount of oxygen in the blood falls below normal levels, leading to hypoxia. It is recommended to seek medical attention if the oxygen saturation levels drop below 92%, and immediate attention is required if it falls to 88% or lower. Monitoring oxygen saturation levels using a pulse oximeter is essential for individuals at risk of hypoxia.
The Effects of Low Oxygen Levels on the Body
When your body experiences low oxygen levels, a condition called hypoxemia, you may feel a variety of symptoms. These symptoms can vary depending on the severity and duration of the hypoxemia.
Some common symptoms of hypoxemia include:
– Shortness of breath: This is often one of the first and most noticeable symptoms of low oxygen levels. You may feel like you can’t catch your breath, even when you’re not exerting yourself.
– Headache: A headache is a common symptom of hypoxemia, especially if the low oxygen levels are chronic.
– Confusion or restlessness: Low oxygen levels can affect your brain function, leading to confusion or restlessness.
– Rapid heartbeat: Your heart may beat faster than usual as it tries to compensate for the lack of oxygen.
– Chest pain: In some cases, hypoxemia can cause chest pain or discomfort.
Other symptoms of hypoxemia can include fatigue, dizziness, and cyanosis (a bluish tint to the skin or lips).
It’s important to note that not everyone experiences the same symptoms of hypoxemia, and some people may not experience any symptoms at all, especially if the low oxygen levels are mild or brief. If you suspect that you may have low oxygen levels, it’s important to seek medical attention riht away to determine the cause and receive appropriate treatment.
Normal Oxygen Levels by Age
Oxygen saturation levels, measured by pulse oximetry, are an important indicator of respiratory function. A normal oxygen level for an adult is considered to be between 95 to 100 percent. However, oxygen level can vary depending on the age of the individual.
For children, normal oxygen saturation levels range from 95 to 100 percent, similar to adults. It is important to note that premature infants may have lower oxygen saturation levels, around 90 to 95 percent, as their lungs are still developing.
As individuals age, normal oxygen saturation levels may decrease slightly. For people over 70 years of age, oxygen levels closer to 95 percent are considered normal. This is due to the natural aging process, as well as potential underlying health conditions that can affect respiratory function.
It is important to monitor oxygen saturation levels in individuals with respiratory conditions, such as chronic obstructive pulmonary disease (COPD) or asthma, as well as thoe with COVID-19 or other respiratory illnesses. If oxygen levels fall below 95 percent, medical attention may be required.
Normal oxygen saturation levels range from 95 to 100 percent for both adults and children, with slightly lower levels considered normal for those over 70 years of age.
Raising Oxygen Levels Quickly
In order to quickly increase your oxygen level, there are a few simple methods you can try. These include:
1. Deep Breathing Exercises: Taking deep breaths and holding them for a few seconds before exhaling can help increase the amount of oxygen in your body.
2. Physical Exercise: Engaging in physical activity such as jogging or brisk walking can get your heart rate up and increase your respiratory rate, which in turn increases the amount of oxygen in your bloodstream.
3. Oxygen Therapy: Oxygen therapy involves using a machine that delivers oxygen directly to your lungs. This method is typically used for people with respiratory conditions, but can be used to increase oxygen levels in healthy individuals as well.
4. Increase Your Water Intake: Drinking plenty of water can help increase the amount of oxygen in your bloodstream. This is because water helps to thin your blood, allowing it to carry more oxygen to your body’s tissues.
5. Open Your Windows or Go Outside: As mentioned earlier, opening your windows or going outside for a walk can increase the amount of oxygen that your body brings in, which increases your overall blood oxygen level.
There are many simple and effective ways to increase your oxygen level quickly. By practicing deep breathing exercises, engaging in physical activity, using oxygen therapy, increasing your water intake, and getting some fresh air, you can boost your oxygen levels and improve your overall health and well-being.

Which Finger is Most Suitable for Using an Oximeter?
When it comes to measuring arterial oxygen saturation levels using an oximeter, the finger that is generally considered to be the best is the right middle finger. This is because the arteries in the middle finger are closer to the surface of the skin and less likely to be affected by other factors such as cold temperatures or peripheral vascular disease.
That beig said, the right thumb is also often used as an alternative, as it also has a high level of accuracy in reflecting arterial oxygen saturation. It is important to note, however, that the accuracy of readings can also depend on the quality and calibration of the oximeter device being used.
While the right middle finger is generally considered to be the best finger for oximeter readings, the right thumb can also provide accurate results. It is recommended to consult with a healthcare professional for guidance on proper oximeter usage and interpretation of results.
Here are some key points to remember:
– The right middle finger is generally considered the best for oximeter readings due to the proximity of the arteries to the skin surface.
– The right thumb can also provide accurate results.
– Quality and calibration of the oximeter device can affect accuracy.
– It is important to consult with a healthcare professional for guidance on proper oximeter usage and interpretation of results.
How Long Should I Keep My Finger in an Oximeter?
When using a pulse oximeter, it is important to keep your finger in place for at least one minute to ensure a steady reading. If the reading continues to fluctuate, it may be necssary to keep your finger in place for longer until the reading stabilizes. Once the reading has remained consistent for at least five seconds, record the highest result. It is important to be aware of the heart rate and oxygen level readings and to identify them correctly. Here are some tips to ensure accurate readings:
– Keep your finger still and avoid moving it during the reading
– Make sure the pulse oximeter is securely attached to your finger
– Avoid using the pulse oximeter in cold temperatures, as this can affect the accuracy of the reading
– Check the battery level of the pulse oximeter to ensure accurate readings
– If you are using the pulse oximeter to monitor a medical condition, follow your healthcare provider’s instructions for use and interpreting the results.
By following these guidelines, you can ensure accurate and reliable readings from your pulse oximeter.
Conclusion
As we have seen, a pleth is a graphical display of the pulse oximeter signal over time, and it can provide valuable information about a patient’s oxygen saturation levels. In particular, the relative variability in the pleth during respiratory cycles, as measured by PVi, can be used as a dynamic indicator of fluid responsiveness in select populations of mechanically ventilated adult patients.
It is important to note that a normal level of oxygen saturation is usually 95% or higher, and that values betwen 95% and 100% are typical for most healthy individuals. However, some people with chronic lung disease or sleep apnea may have normal levels around 90%, and oxygen saturation levels can also be lower for those living at higher altitudes.
A good pleth can provide valuable information about a patient’s oxygen saturation levels, and PVi can be used as a dynamic indicator of fluid responsiveness in select populations of mechanically ventilated adult patients. By carefully monitoring and interpreting pleth data, healthcare providers can help ensure that their patients are receiving the best possible care.
