Amorphous sediment refers to the presence of shapeless or formless crystals in the urine. While it may sound concerning, in most cases, the presence of amorphous crystals is of little clinical significance. These crystals are typically formed due to a combination of factors, including decreased urine volume, changes in urine pH, and the presence of certain substances in the diet.
One common type of amorphous sediment is composed of uric acid. Uric acid is a byproduct of the breakdown of purines, which are found in certain foods, particularly meat. When there is an excess of uric acid in the urine, it can crystallize and contribute to the formation of amorphous sediment.
Another type of amorphous sediment contains calcium and magnesium phosphate. This type of sediment is commonly found in urine with a pH above 6.5. It is often associated with certain dietary factors, such as the consumption of dairy products that are rich in calcium.
It is important to note that the presence of amorphous sediment does not necessarily indicate a urinary tract infection. While sediment in the urine can be a sign of various infections, including those affecting the urinary tract, it can also be caused by other factors such as kidney stones, vaginal bacteria, yeast infections in both men and women, prostatitis, and even parasites.
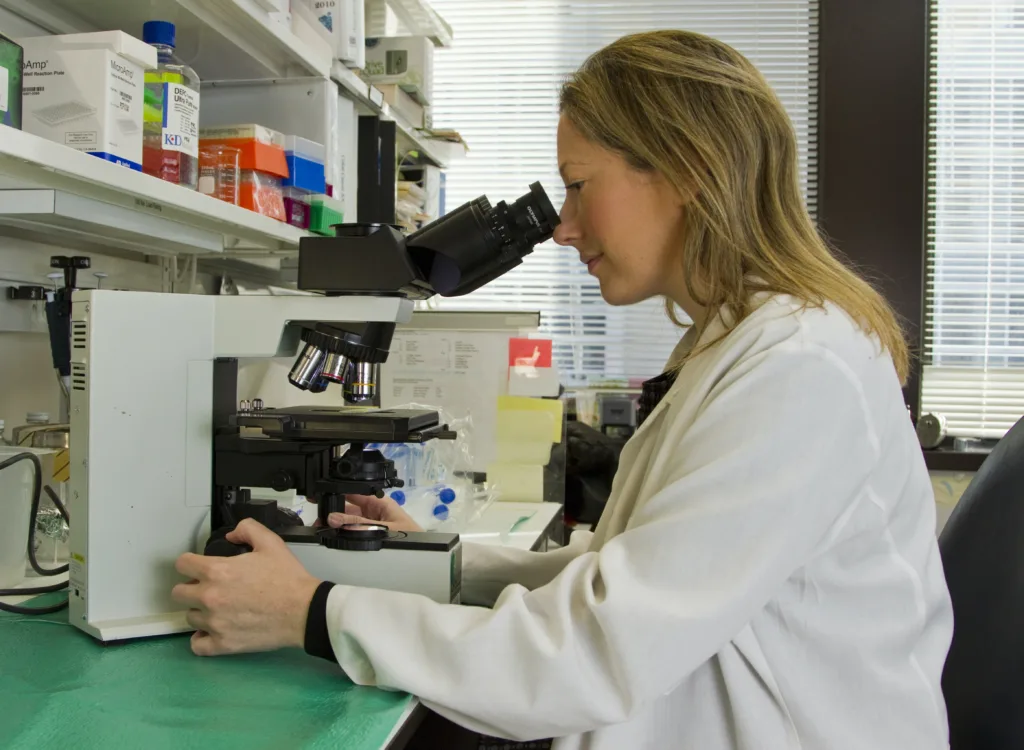
To identify the type of crystals present in the sediment, laboratory tests are conducted. The shape of the crystals can be observed under a microscope, allowing for their identification. In some cases, the crystals may have no identifiable shape and appear as amorphous.
The pH, or acidity, of the urine can also contribute to the formation of specific types of crystals. For example, urine with a higher pH is more likely to have amorphous phosphate crystals, while a lower pH may promote the formation of uric acid crystals.
The presence of amorphous sediment in the urine is generally of little clinical significance. It is often caused by factors such as decreased urine volume, changes in urine pH, and the consumption of certain foods. While it can be a sign of various infections, it is not always indicative of an underlying medical condition. If you notice sediment in your urine or have concerns about your urinary health, it is important to consult a healthcare professional for further evaluation and guidance.
What Causes Amorphous Sediment?
Amorphous sediment in urine can be caused by a variety of factors. Here are some key causes:
1. Decreased urine volume: When the body doesn’t produce enough urine, it can lead to the formation of amorphous sediment. This can occur due to dehydration, certain medical conditions, or medications that reduce urine output.
2. Changes in urine pH: The pH level of urine can influence the formation of amorphous sediment. Urine that is too acidic or too alkaline can promote the precipitation of substances, such as uric acid or calcium, leading to the formation of amorphous crystals.
3. Diet: The type of diet a person follows can also contribute to the formation of amorphous sediment. Consuming large quantities of foods rich in uric acid, such as meat and seafood, can increase the likelihood of uric acid crystals forming in the urine. Similarly, a diet high in calcium-rich foods, like dairy products, can result in the presence of calcium crystals.
4. Medications: Certain medications, such as diuretics, can alter urine composition and increase the risk of amorphous sediment formation. It is important to consult with a healthcare professional if you suspect that a medication may be causing this issue.
5. Underlying medical conditions: In some cases, amorphous sediment may be a sign of an underlying medical condition. Conditions that affect urine composition, such as kidney stones or urinary tract infections, can lead to the presence of amorphous crystals in the urine.
It’s worth noting that the presence of amorphous crystals in urine is generally of little clinical significance. However, if you have concerns about your urine sediment or experience other urinary symptoms, it is important to consult with a healthcare professional for proper evaluation and guidance.
Is Amorphous Normal In Urine?
The presence of amorphous phosphate crystals in urine is considered normal and is not typically a cause for concern. These crystals are composed of calcium and magnesium phosphate and are commonly found in urine that has a pH level above 6.5.
Here are some key points about amorphous phosphate crystals in urine:
1. Composition: Amorphous phosphate crystals are made up of calcium and magnesium phosphate. They are called “amorphous” because they lack a defined shape or structure.
2. Appearance: These crystals may appear as small, colorless or slightly yellowish granules or clumps in urine. They are often seen under a microscope during routine urine analysis.
3. pH and solubility: Amorphous phosphate crystals tend to form in urine that has an alkaline pH (above 6.5), which means it is more basic than acidic. They dissolve easily in acidic urine but can precipitate and accumulate in alkaline urine.
4. Clinical significance: In most cases, the presence of amorphous phosphate crystals in urine is considered benign and does not indicate any underlying medical condition. They are commonly seen in healthy individuals.
5. Factors influencing formation: Several factors can contribute to the formation of amorphous phosphate crystals, including diet, hydration status, and medication use. For example, a diet rich in calcium or magnesium may increase the likelihood of their presence.
6. Importance of interpretation: It is important to consider other factors and clinical context when evaluating urine test results. The presence of amorphous phosphate crystals alone does not necessarily indicate a health problem. Healthcare professionals will consider other urine parameters and patient symptoms to make an accurate diagnosis.
The presence of amorphous phosphate crystals in urine is generally considered normal and does not typically indicate any significant clinical issue. However, it is always advisable to consult a healthcare professional for a comprehensive evaluation and interpretation of urine test results.
What Does Sediment In Urine Mean?
Sediment in urine refers to the presence of particles or material that are not typically found in healthy urine. While sediment can indicate a urinary tract infection (UTI), it can also be caused by various other factors. Here are some possible reasons for the presence of sediment in urine:
1. Urinary tract infection (UTI): A common cause of sediment in urine is a bacterial infection in the urinary tract, which can affect the bladder, urethra, or kidneys. Bacteria, white blood cells, and other inflammatory cells may be present in the urine, leading to sediment.
2. Kidney infection: A more severe form of UTI, a kidney infection can also cause sediment in urine. In addition to bacteria and inflammatory cells, kidney infections may result in the presence of blood or pus in the urine.
3. Bladder infection: Infections specifically targeting the bladder can cause sediment in urine. Bacteria, white blood cells, and mucus may be present, leading to the appearance of sediment.
4. Kidney stones: Sediment can be a result of the presence of kidney stones in the urinary tract. These solid masses can cause blood in the urine and the release of particles, contributing to sediment formation.
5. Vaginal bacteria: In some cases, vaginal bacteria can contaminate urine during sample collection, leading to the appearance of sediment. This is more common in women and can be prevented by carefully cleaning the genital area before urine collection.
6. Yeast infections: Both men and women can experience yeast infections, which may result in sediment in urine. Yeast cells and their byproducts can be present in the urine, leading to the formation of sediment.
7. Prostatitis: Inflammation of the prostate gland, known as prostatitis, can cause sediment in urine for males. In addition to bacteria and inflammatory cells, prostatic secretions may contribute to sediment formation.
8. Parasitic infections: Certain parasites, such as Schistosoma or Trichomonas, can infect the urinary tract and result in sediment in urine. These infections are less common but should be considered as a possible cause.
It is important to note that the presence of sediment in urine does not always indicate an infection. It can be a sign of various conditions, and further evaluation by a healthcare professional is necessary to determine the underlying cause.
What Does Amorphous Urinalysis Mean?
Amorphous urinalysis refers to the presence of amorphous crystals in the urine sample. Amorphous crystals are microscopic substances that lack a definite shape or structure. When urine is analyzed under a microscope, these crystals appear as shapeless particles or granules.
Amorphous crystals can be composed of various substances, including phosphates, urates, oxalates, or carbonates. The specific composition of amorphous crystals can provide valuable information about a person’s health and potential underlying conditions.
The presence of amorphous urinalysis can indicate several things:
1. pH imbalance: The acidity or alkalinity of urine plays a role in the formation of crystals. Amorphous urinalysis can occur when the pH level of urine is outside the normal range. For example, alkaline urine (high pH) may result in the formation of amorphous phosphates, while acidic urine (low pH) can lead to amorphous urates.
2. Dehydration: Insufficient fluid intake can lead to concentrated urine, which may increase the likelihood of amorphous crystal formation. Inadequate hydration can also contribute to the formation of other types of crystals, such as calcium oxalate or cystine.
3. Kidney stones: In some cases, amorphous urinalysis may be associated with the presence of kidney stones. This is particularly true if other crystal types, such as calcium oxalate or uric acid crystals, are also present in the urine.
It is important to note that amorphous crystals themselves are usually not considered a significant health concern. However, their presence may indicate an underlying issue that needs further evaluation, such as kidney function or urinary tract health.
To determine the exact composition and significance of amorphous urinalysis, additional tests or evaluation by a healthcare professional may be necessary.
Conclusion
Amorphous sediment refers to the presence of shapeless crystals in urine. While generally of little clinical significance, the formation of amorphous crystals is influenced by factors such as decreased urine volume, changes in urine pH, and the consumption of certain foods like meat (leading to uric acid crystals) or dairy products (resulting in calcium crystals). Amorphous phosphate crystals, composed of calcium and magnesium phosphate, are particularly common and usually not medically worrisome. The presence of sediment in urine can be indicative of various conditions, including urinary tract infections, kidney infections, bladder infections, kidney stones, vaginal bacteria or yeast infections, prostatitis, and even parasites. Laboratory tests can help identify the specific type of crystals present, and the pH level of urine plays a role in their formation. while the presence of amorphous sediment may raise concerns, it is important to consider other clinical factors and consult with a healthcare professional for an accurate diagnosis and appropriate treatment if necessary.
