In the intricate system of our circulatory system, blood cells play a vital role in maintaining our overall health and well-being. Among these blood cells, there are specific types that are essential for vessel repair and clotting. Let’s delve into the fascinating world of these cells and explore their functions in more detail.
One of the key players in clotting is the platelet, also known as thrombocyte. Despite their small size, platelets are mighty in their ability to form clumps and plug holes in damaged blood vessels to prevent excessive bleeding. They are actually fragments of larger cells called megakaryocytes, and their primary job is blood clotting.
When an injury occurs, platelets release molecules into the bloodstream that initiate the clotting process. These molecules, known as clotting factors, have a crucial role in activating the necessary components for clot formation. One such vital clotting factor is fibrin, a protein that forms a long, thin, and sticky mesh when activated.
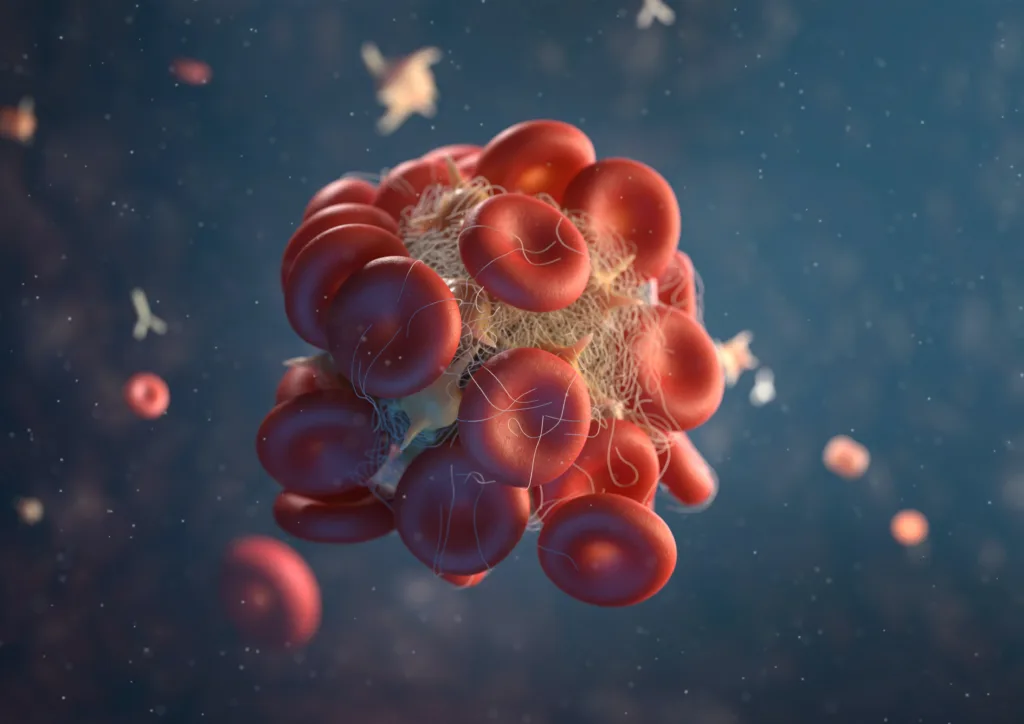
Once fibrin is turned on, it intertwines with the platelet plug, creating a strong network that holds everything together. This mesh, known as a fibrin clot, acts as a barrier, preventing further blood loss and allowing the damaged vessel to undergo the necessary repair processes. As the clot dries, it forms a scab, aiding in the healing of the wound.
Clotting is a complex process that involves the coordination of various blood cells and clotting factors. Platelets work hand in hand with clotting factors, such as prothrombin and thrombin, to ensure the formation of a stable and effective clot. Without these essential components, our bodies would struggle to stop bleeding and heal wounds efficiently.
Apart from platelets, other blood cells also contribute to vessel repair and clotting. For instance, white blood cells, or leukocytes, play a crucial role in fighting off infections and aiding in the healing process. They help remove any foreign substances or bacteria that may have entered the body through the damaged vessel.
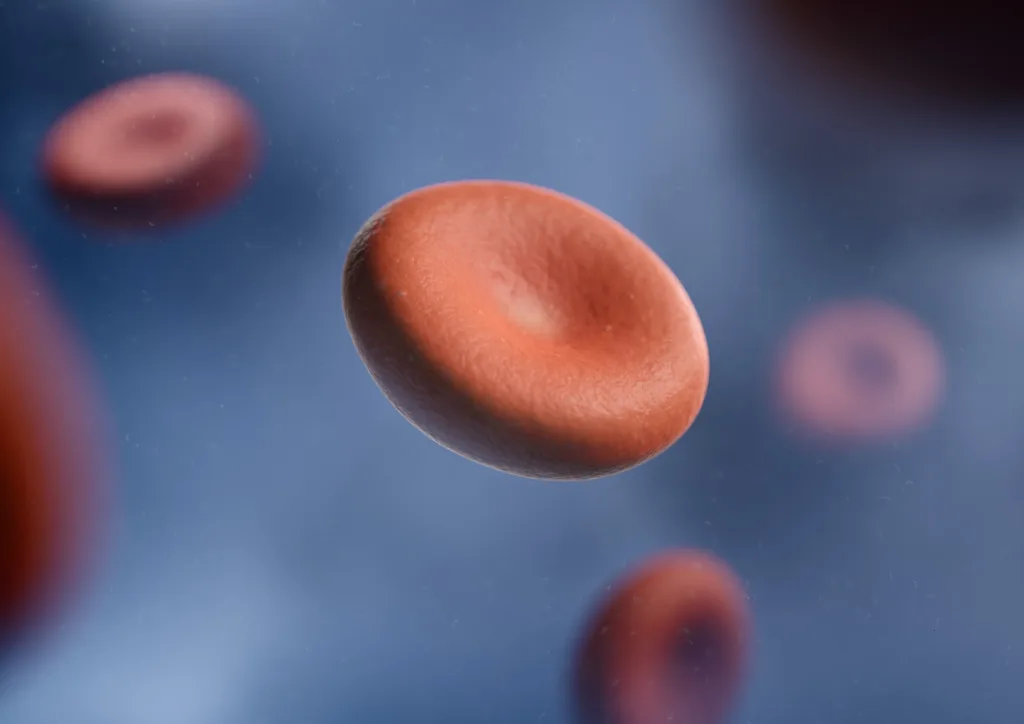
Red blood cells, or erythrocytes, also have a role in clotting. Although they are not directly involved in the clot formation process, their presence is essential for maintaining the necessary oxygen supply to injured tissues. Oxygen is crucial for the functioning and repair of cells, and red blood cells ensure its transport to the damaged site.
Blood cells, especially platelets, are indispensable for vessel repair and clotting. Platelets form clumps and create a plug to stop bleeding, while clotting factors like fibrin form a mesh that reinforces the plug, resulting in a stable clot. The collaboration between platelets, clotting factors, and other blood cells is vital for effective clot formation and vessel repair. Understanding the intricate mechanisms of these cells allows us to appreciate the remarkable capabilities of our bodies in healing and maintaining our well-being.
What Cells Are Necessary For Blood Clotting?
Blood clotting, also known as coagulation, is a crucial process that helps prevent excessive bleeding when a blood vessel is damaged. Several types of cells and proteins work together to form a blood clot. The main cells involved in blood clotting are:
1. Platelets (Thrombocytes): Platelets are small, disk-shaped cells that circulate in the blood. When a blood vessel is injured, platelets form clumps and adhere to the damaged site. They release chemicals that attract more platelets and help in the formation of a plug to stop bleeding.
2. Red Blood Cells (Erythrocytes): Although red blood cells are not directly involved in the clotting process, they play a role in forming a stable clot. Red blood cells help in creating a mesh-like structure that strengthens the clot and helps it adhere to the damaged vessel wall.
3. White Blood Cells (Leukocytes): White blood cells are part of the immune system and are not directly involved in clot formation. However, they play a role in the later stages of clotting by removing debris and fighting off potential infections that may occur at the site of injury.
4. Coagulation Factors: Coagulation factors are proteins in the blood that work together to promote clot formation. There are thirteen different coagulation factors (numbered I to XIII), and each plays a specific role in the clotting cascade. These factors help convert a protein called fibrinogen into fibrin, which forms a mesh-like network to strengthen the clot.
Platelets are the primary cells responsible for initiating clot formation. However, red blood cells, white blood cells, and various coagulation factors also play important roles in the complex process of blood clotting.
What Cells Are Necessary For Vessel Repair And Clotting Neutrophils?
In the process of vessel repair and clotting, there are several types of cells involved, including neutrophils. Here is a detailed explanation of the cells necessary for vessel repair and clotting:
1. Platelets: Platelets, also known as thrombocytes, are small cell fragments found in the blood. They play a crucial role in forming blood clots, which is a crucial step in vessel repair. When there is damage to a blood vessel, platelets become activated and aggregate at the site of injury to form a plug. This plug helps to stop bleeding and initiates the clotting process.
2. Neutrophils: Neutrophils are a type of white blood cell and are part of the immune system. While their primary function is to fight off infections and foreign substances, they also play a role in vessel repair and clotting. Neutrophils are attracted to the site of injury by chemical signals released during the clotting process. Once at the site, they release substances that help to break down any dead tissue and bacteria, promoting healing and preventing infection.
3. Endothelial cells: Endothelial cells line the inner surface of blood vessels and play a crucial role in vessel repair. When a blood vessel is damaged, these cells produce substances that help to activate platelets and initiate the clotting process. Additionally, endothelial cells release chemicals that promote the growth of new blood vessels, called angiogenesis, to aid in the repair process.
4. Fibroblasts: Fibroblasts are connective tissue cells that are involved in the later stages of vessel repair. Once the clot has formed and the initial inflammation subsides, fibroblasts migrate to the site of injury and produce collagen, a protein that provides structural support to the repaired vessel. Collagen helps to strengthen the vessel wall and promote its proper function.
These cells work together in a coordinated manner to ensure effective vessel repair and clotting. Platelets initiate the clotting process, neutrophils help to clear debris and prevent infection, endothelial cells activate platelets and promote angiogenesis, and fibroblasts contribute to the structural integrity of the repaired vessel.
Which Blood Cells Are Involved In Clotting Damaged Blood Vessels?
When a blood vessel is damaged, several blood cells are involved in the process of clotting. The main cells responsible for clotting are platelets, also known as thrombocytes. Platelets are small, disc-shaped cells that circulate in the blood. When there is an injury, platelets are activated and begin to stick together at the site of the damage.
In addition to platelets, clotting factors are also crucial for the formation of a blood clot. These clotting factors are proteins present in the blood that work together to form a clot. One important clotting factor is fibrinogen, which is converted into fibrin during the clotting process.
The process of clotting begins with the release of molecules by platelets. These molecules help activate clotting factors, including fibrinogen. Once activated, fibrinogen is converted into fibrin, which forms a mesh-like structure to hold the platelets together at the site of the injury. This fibrin clot helps to seal the damaged blood vessel and prevent further bleeding.
The blood cells involved in clotting damaged blood vessels are platelets, along with the clotting factors, particularly fibrinogen. These cells and proteins work together to form a fibrin clot, which plays a crucial role in stopping bleeding and initiating the healing process.
Which Cells Help To Form A Clot When We Get A Wound?
Platelets, also known as thrombocytes, play a crucial role in forming blood clots when we get a wound. These small, disk-shaped cells are produced in the bone marrow and circulate in the blood. When a blood vessel is damaged, platelets are immediately activated and rush to the site of injury.
Here’s a step-by-step breakdown of how platelets help form a clot:
1. Adhesion: Platelets adhere to the damaged blood vessel wall, sticking to the exposed collagen fibers.
2. Activation: Upon adhesion, platelets undergo a process called activation, where they change shape and release various chemicals and molecules. These substances help recruit more platelets to the site and promote clot formation.
3. Aggregation: Activated platelets bind together, forming a clump or aggregate. This aggregation is facilitated by a protein called fibrinogen, which acts as a glue-like substance, binding platelets together.
4. Secretion: Platelets release granules containing substances such as clotting factors, growth factors, and chemicals that promote inflammation. These factors help in further recruitment of platelets and initiate the clotting cascade.
5. Clotting cascade: The released clotting factors trigger a complex series of biochemical reactions known as the clotting cascade. This cascade involves the activation of various proteins, ultimately leading to the conversion of fibrinogen into fibrin.
6. Fibrin mesh formation: Fibrin, a thread-like protein, forms a mesh-like network around the platelet aggregate. This fibrin mesh traps more platelets, red blood cells, and plasma, forming a solid clot.
7. Scab formation: As the clot dries, it forms a scab, protecting the wound and promoting healing. The scab helps prevent further bleeding and acts as a barrier against infection.
It is important to note that while platelets initiate clotting, other proteins and cells, such as clotting factors and red blood cells, are also involved in the clotting process. However, platelets play a central role in the initial stages of clot formation.
Conclusion
Blood cells play crucial roles in maintaining the overall health and functioning of our bodies. Red blood cells, or erythrocytes, transport oxygen to all our organs and tissues, ensuring their proper functioning. White blood cells, or leukocytes, are essential for our immune system, defending us against harmful pathogens and infections. Lastly, platelets, or thrombocytes, are responsible for blood clotting, preventing excessive bleeding and aiding in vessel repair. Each type of blood cell has its unique characteristics and functions, working together to support our overall well-being. Understanding the role of these blood cells helps us appreciate the complexity and importance of our circulatory system.
