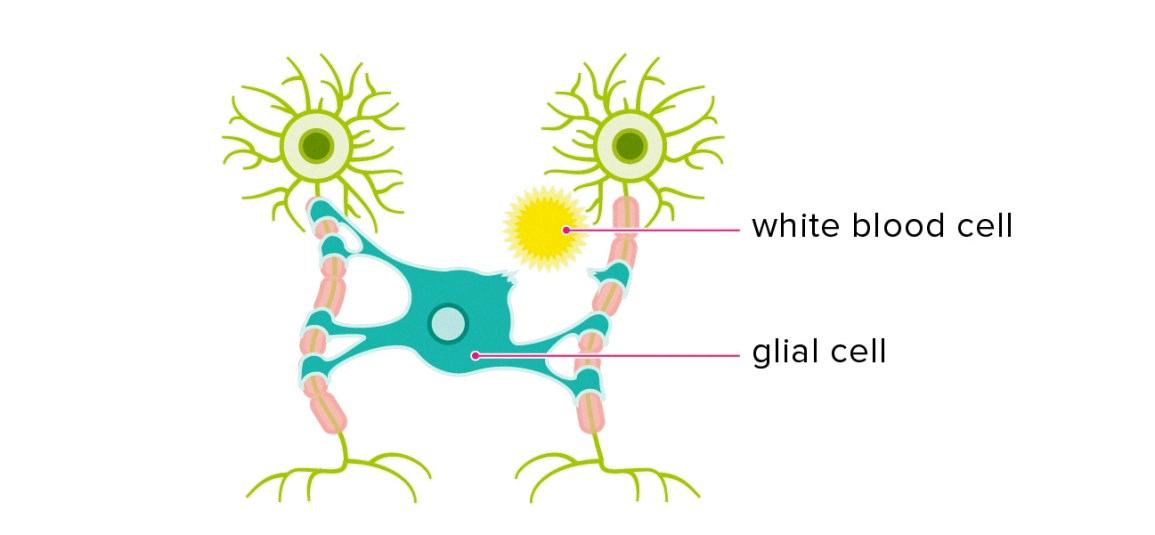
Multiple sclerosis (MS) is a chronic and progressive neurological disorder that affects the central nervous system (CNS). It is a disease that affects the myelin, whih is the protective coating that surrounds the nerve fibers in the CNS. The damage to the myelin causes the nerves to become disrupted, leading to symptoms that can range from mild to severe.
One of the most common questions asked by individuals diagnosed with MS and their loved ones is, “Does MS kill you?” The answer to this question is not a simple one.
MS is not typically fatal, but it can lead to complications that can be life-threatening. These complications can include respiratory issues, infections, and injuries due to mobility issues.
Respiratory issues are a major concern for individuals with MS, particularly those in the final stages of the disease. MS can weaken the muscles that control the lungs, making it difficult to breathe. This can lead to pneumonia, which can be life-threatening.
Infections are also a concern for individuals with MS. The disease can weaken the immune system, making it more difficult for the body to fight off infections. This can lead to complications such as sepsis, which can be fatal.
Mobility issues are another concern for individuals with MS. As the disease progresses, it can lead to muscle weakness, spasticity, and balance problems, which can increase the risk of falls and injuries. These injuries can be particularly dangerous for older individuals or those with other health conditions.
It is important to note that the life expectancy for individuals with MS is typically around 5 to 10 years lower than average, but this gap appears to be getting smaller as treatments improve. Additionally, many individuals with MS are able to lead long, active, and healthy lives with the right care and support.
There are four stages of MS: clinically isolated syndrome (CIS), relapsing-remitting MS (RRMS), secondary-progressive MS (SPMS), and primary-progressive MS (PPMS). The progression of the disease can vary greatly from person to person, and it is difficult to predict how the disease will progress.
While MS is not typically fatal, it can lead to complications that can be life-threatening. It is important for individuals with MS to work closely with their healthcare team to manage their symptoms and prevent complications. With the right care and support, many individuals with MS are able to lead long, active, and healthy lives.
Life Expectancy with Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic and progressive neurological disorder that affects the central nervous system. The life expectancy of people with MS is generally slightly lower than that of the general population. According to several studies, individuals with MS have an average life expectancy that is around 5 to 10 years lower than the general population. However, it is important to note that this gap seems to be decreasing over time, possibly due to advancements in medical treatments and improvements in overall healthcare.
It is also worth mentioning that life expectancy can vary depending on vaious factors, including the individual’s age at diagnosis, the type and severity of MS, and overall health status. Additionally, managing MS symptoms, following a healthy lifestyle, and adhering to treatment plans can help improve quality of life and potentially increase life expectancy. Therefore, it is important for individuals with MS to work closely with their healthcare providers to develop and maintain an effective and personalized treatment plan.

Source: folks.pillpack.com
Living with Multiple Sclerosis: Can You Lead a Normal Life?
Many people with multiple sclerosis (MS) are able to live normal lives with the right care and support. MS is a chronic condition that affects the central nervous system, leading to a range of symptoms such as fatigue, muscle weakness, and difficulties with balance and coordination. However, with proper treatment and management, many people with MS are able to lead fulfilling and active lives.
The key to living well with MS is to work closely with healthcare professionals to develop an individualized treatment plan that addresses your specific symptoms and needs. This may include medications to manage symptoms or slow the progression of the disease, physical therapy to improve strength and mobility, and cognitive therapy to address any cognitive changs that may occur.
In addition to medical treatment, many people with MS benefit from making lifestyle changes such as eating a healthy diet, getting regular exercise, and managing stress. It’s also important to build a strong support network of family, friends, and healthcare professionals who can provide emotional support and practical assistance when needed.
While MS can certainly impact your daily life, it’s important to remember that many people with the condition are able to live full and active lives. With the right care, support, and attitude, there’s no reason why you can’t continue to pursue your goals and dreams.
The Effects of Multiple Sclerosis on Mortality
MS itself is not a direct cause of death. However, the disease can lead to complications that can be life-threatening. Respiratory issues are the major cause of sickness and death in people in the final stages of MS. This is because MS can weaken the muscles that control the lungs, making it difficult to breathe. Additionally, MS can cause spasticity or an increase in stiffness and resistance as a muscle is moved, impairing movement and causing pain and other problems. These complications can lead to pneumonia, respiratory failure, and other serious conditions that can ultimately result in death. It is important for individuals with MS to monitor teir symptoms closely and seek medical attention if they experience any respiratory problems or other complications.
The Four Stages of Multiple Sclerosis
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system, causing damage to the myelin covering on nerves in the brain or spinal cord. MS is a progressive disease, which means that symptoms may worsen over time. There are four stages of MS, each with its own unique characteristics and symptoms.
The first stage is called Clinically Isolated Syndrome (CIS). This is the initial episode of symptoms caused by inflammation and damage to the myelin covering on nerves in the brain or spinal cord. The symptoms of CIS can vary widely and may include numbness, tingling, weakness, or loss of vision. Not everyone who experiences CIS will go on to develop MS.
The second stage is Relapsing-Remitting MS (RRMS). This is the most common form of MS, affecting around 85% of those diagnosed with MS. In this stage, people experience relapses, or flare-ups, of symptoms. These relapses are followed by periods of remission, during which symptoms may improve or disappear entirely. RRMS can last for many years, and some people may never progress to the later stages of MS.
The third stage is Secondary-Progressive MS (SPMS). This stage typically follows RRMS, and involves a gradual worsening of symptoms, with or without relapses. In SPMS, symptoms may become more severe and may not improve during periods of remission. This stage can be challenging to manage and may require more aggressive treatment.
The final stage is Primary-Progressive MS (PPMS). This is the least common form of MS, affecting around 10-15% of those diagnosed with MS. In PPMS, symptoms gradually worsen from the onset of the disease, without periods of remission. This stage can be paticularly challenging to manage and may require a more individualized approach to treatment.
MS is a complex and progressive disease that can be challenging to manage. Understanding the four stages of MS can help those affected to better understand their symptoms and plan for the future. It is important to work closely with a healthcare provider to develop a personalized treatment plan that addresses individual needs and goals.
The Age Range of Onset for Multiple Sclerosis
Multiple Sclerosis (MS) is a disease that affects the central nervous system. While MS can occur at any age, the onset usually occurs around 20 and 40 years of age. However, it’s important to note that younger and older people can also be affected by MS. Women are more than two to three times as likely as men are to have relapsing-remitting MS. It’s essential to consult a healthcare professional if you experience any symptoms or concerns related to MS. Early diagnosis and treatment can help manage symptoms and improve quality of life.

Source: people.com
The Rate of Progression of Multiple Sclerosis
The progression of multiple sclerosis (MS) can vary greatly between individuals, as the disease affects each person differently. Some people experience a more aggressive form of MS that progresses rapidly, while others may experience a more mild form of the disease that progresses slowly over time. It’s important to note that MS is a chronic condition, which means that symptoms can come and go throughout a person’s lifetime.
MS symptoms may develop abruptly, within hours or days, during what is known as an “attack” or “relapse”. These attacks typically reach thir peak within a few days at most and then resolve slowly over the next several days or weeks, so that a typical relapse will be symptomatic for about eight weeks from onset to recovery.
In terms of the overall progression of MS, the disease can progress in a few different ways. Some people may experience a steady progression of symptoms over time, while others may experience periods of relapse and remission, where symptoms flare up and then subside. There are also some medications and treatments available that may help slow the progression of MS and manage symptoms.
Ultimately, the speed at which MS progresses can depend on a variety of factors, including the individual’s age, gender, overall health, and the specific type of MS they have. It’s important for individuals with MS to work closely with their healthcare team to develop a personalized treatment plan that can help manage symptoms and slow the progression of the disease.
Can People with Multiple Sclerosis Drive?
Many people with MS can drive normally. However, some may require adaptive equipment such as hand controls or modifications to the vehicle to make it easier to operate. It is important to note that driving with MS requires careful consideration and evaluation to ensure safety on the road. Some people may experience symptoms such as fatigue, cognitive difficulties, or vision problems that can impact teir ability to drive safely. In some cases, it may be necessary to stop driving altogether. To determine if it is safe for a person with MS to drive, it is recommended to get evaluated by a driving rehabilitation specialist who can assess their abilities and recommend any necessary adaptations or modifications to ensure safety on the road.
The Effects of Drinking Alcohol with Multiple Sclerosis
It is generally not recommended to drink alcohol if you have Multiple Sclerosis (MS). Alcohol can worsen some of the common symptoms of MS, such as unsteadiness, memory problems, and bladder issues. Even a small amount of alcohol can make these symptoms worse. If you have a lot of difficulty with balance, thinking, or memory symptoms, it may be best to avoid alcohol altogether. Additionally, alcohol can interfere with sleep, whch can also worsen MS symptoms. It is important to talk to your doctor about the potential risks and benefits of drinking alcohol with MS, as individual factors such as age, medication use, and overall health can also play a role in determining whether alcohol consumption is safe for you.
Can Multiple Sclerosis Be Inherited?
Multiple sclerosis (MS) is not a condition that someone is born with. MS is a chronic autoimmune disease that affects the central nervous system, and it typically develops in adulthood. While the exact cause of MS is not fully understood, it is believed to be a combination of environmental and genetic factors. Although MS is not directly inherited, research has shown that people who have a family member with MS are more likely to develop the condition themselves. However, the chance of developing MS as a result of genetics is relatively low, estimated to be around 2 to 3 in 100 for siblings or children of someone with MS. whle genetics can play a role in the development of MS, it is not a condition that someone is born with.

Source: latimes.com
The Final Stages of Multiple Sclerosis Before Death
As Multiple Sclerosis (MS) progresses, individuals may experience a range of symptoms that can become increasingly severe in the final stages of the disease. These symptoms can include difficulty with balance, coordination, and posture, wich can make it challenging to walk or stand. Limited mobility or paralysis may also occur, making it difficult for individuals to perform daily activities such as dressing, bathing, or using the restroom without assistance. In some cases, individuals may develop blood clots or pressure sores due to lack of mobility and may require specialized medical care. The final stages of MS can be particularly challenging for both the individual and their loved ones, as they may experience significant physical and emotional changes. It is important to work closely with healthcare providers to manage symptoms and provide support during this time.
The Final Stages of Multiple Sclerosis
In the final stages of Multiple Sclerosis (MS), more severe symptoms and complications may develop. These symptoms can vary from person to person, but some common ones include difficulty breathing, limited mobility or paralysis, and speech complications.
Difficulty breathing can occur due to weakened muscles in the chest and diaphragm, making it harder to breathe on one’s own. This may require the use of a ventilator or other respiratory support.
Limited mobility or paralysis can occur due to nerve damage, leading to difficulty walking or being unable to move certain parts of the body. Some individuals may require assistive devices such as wheelchairs or other mobility aids.
Speech complications can occur due to muscle weakness, fatigue, and difficulty with coordination of the mouth and throat muscles. This can make it difficult to speak clearly or communicate effectively.
Other symptoms that may occur in the final stages of MS include cognitive impairment, bowel and bladder dysfunction, and seizures. It’s important to work with a healthcare team to manage symptoms and provide the best posible care for individuals with MS in the final stages of the disease.
The Symptoms of End Stage Multiple Sclerosis
End-stage multiple sclerosis (MS) can vary greatly from person to person, as MS affects each individual differently. However, there are some common symptoms that are typically seen in end-stage MS.
One of the most common symptoms is severe muscle weakness and atrophy, which can make it difficult or impossible for individuals to move or perform daily activities. This weakness can also lead to feeding difficulties and severe weight loss, which may require the use of a feeding tube.
Another symptom that is often seen in end-stage MS is difficulty breathing due to weakening of the respiratory muscles. This can result in shortness of breath, or even require the use of a ventilator to help with breathing.
As MS progresses, individuals may also experience difficulty with speech or lose the ability to speak altogether. This can be due to weakness in the muscles used for speech, or from damage to the parts of the brain that control speech.
Immobility can lead to pressure sores, which can be at risk of becoming infected. It is important for individuals with end-stage MS to receive proper care and attention to prevent pressure sores from developing and to address any that do occur.
It’s important to note that end-stage MS does not necessarily mean the end of life. Many individuals with MS can live for many years with proper care and support. However, it is also important to discuss end-of-life planning with healthcare providers and loved ones to ensure that the individual’s wishes are respected and that they receive apropriate care throughout their journey with MS.
Can Magnetic Resonance Imaging Detect Multiple Sclerosis?
Brain MRI can detect MS (multiple sclerosis). In fact, MRI has becme the most useful test for the diagnosis of MS. This is because MRI is highly sensitive to changes in the brain that are characteristic of MS. Typically, an MRI of the brain will show lesions in the white matter of the brain, which are located deep in the brain near the fluid spaces (ventricles). These lesions are a hallmark of MS and can be seen even in patients who are not yet showing symptoms. MRI may also be used to monitor the progression of MS and to evaluate the effectiveness of treatments. MRI is a critical tool for the diagnosis and management of MS.
Source: healthline.com
The Relationship Between Multiple Sclerosis and Mental Illness
Multiple Sclerosis (MS) can cause various mental health issues, including but not limited to depression, anxiety, and cognitive impairment. It is estimated that up to 50 percent of MS patients can experience depression, which is three times more common than in the general population. Similarly, anxiety is found in up to 40 percent of MS patients. Cognitive impairment is another common problem that can affect up to 65 percent of MS patients, and this can include difficulties with memory, attention, and concentration. It is important to note that MS does not directly cause mental illness, but it can contribute to or exacerbate existing mental health issues. Therefore, it is essential for MS patients to receive proper mental health care and support, aong with their physical treatment, to manage their overall health and wellbeing.
Common Early Signs of Multiple Sclerosis
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system. The symptoms of MS can vary widely, but there are three early signs that are commonly reported by people who have been diagnosed with the disease. Firstly, vision problems are a common early sign of MS. This can include blurred vision, double vision, or loss of vision in one eye. Secondly, tingling and numbness in the arms, legs, or face can also be an early sign of MS. This symptom is often described as a sensation of pins and needles, and can be mild or severe. pains and spasms are another early sign of MS. This can include muscle stiffness, cramps, and shooting pains. If you are experiencing any of tese symptoms, it is important to seek medical attention to determine the cause and receive appropriate treatment.
Conclusion
While multiple sclerosis (MS) can have a significant impact on a person’s life, it is not typically considered a fatal disease. The average life expectancy for people with MS is only slightly lower than the general population, and advancements in treatment and management have continued to improve outcomes for those living with the disease. However, as MS can weaken the muscles that control the lungs, respiratory issues may become a major cause of illness and death in the lter stages of the disease. It’s important for those with MS to work closely with their healthcare team to manage their symptoms and stay as healthy as possible. With the right care and support, it’s possible to lead a full and active life with MS.
